Existing data sources in clinical epidemiology: Laboratory information system databases in Denmark
| Full article title | Existing data sources in clinical epidemiology: Laboratory information system databases in Denmark |
|---|---|
| Journal | Clinical Epidemiology |
| Author(s) | Arendt, Johan F.H.; Hansen, Anette T.; Ladefoged, Søren A.; Sørensen, Henrik T.; Pedersen, Lars; Adelborg, Kasper |
| Author affiliation(s) | Aarhus University Hospital, Aalborg University Hospital |
| Primary contact | Email: jfba at clin dot au dot dk |
| Editors | Dr. Eyal Cohen |
| Year published | 2020 |
| Volume and issue | 12 |
| Page(s) | 469–75 |
| DOI | 10.2147/CLEP.S245060 |
| ISSN | 1179-1349 |
| Distribution license | Creative Commons Attribution-NonCommercial 3.0 Unported |
| Website | https://www.dovepress.com/existing-data-sources-in-clinical-epidemiology-laboratory-information |
| Download | https://www.dovepress.com/getfile.php?fileID=58155 (PDF) |
Abstract
Routine biomarker results from hospital laboratory information systems (LIS)—covering hospitals and general practitioners—in Denmark are available to researchers through access to the regional Clinical Laboratory Information System Research Database at Aarhus University and the nationwide Register of Laboratory Results for Research. This review describes these two data sources. The laboratory databases have different geographical and temporal coverage. They both include individual-level biomarker results that are electronically transferred from LISs. The biomarker results can be linked to all other Danish registries at the individual level using the unique identifier, the CPR number. The databases include variables such as the CPR number, date and time (hour and minute) of sampling, NPU code, and name of the biomarker, identification code for the laboratory and the requisitioner, the test result with the corresponding unit, and the lower and upper reference limits. Access to the two databases differs since they are hosted by two different institutions. Data cannot be transferred outside Denmark, and direct access is provided only to Danish institutions. It is concluded that access to data on routine biomarkers expands the detailed biological and clinical information available on patients in the Danish healthcare system. The full potential is enabled through linkage to other Danish healthcare registries.
Keywords: biomarkers, database, data resource, laboratory information systems
Data resource basics
Danish healthcare registries
Denmark has a large network of population-based healthcare registries.[1] Several supplementary issues of international medical journals have been devoted to describe these registries to facilitate their use in research.[2][3] The registries contain data on the Danish population of approximately 5.8 millions inhabitants and include data on healthcare contacts, hospital diagnoses, redeemed prescriptions, childbirths, causes of death, and a wide variety of other information. The Civil Registration System and the healthcare system in Denmark have been described in detail elsewhere.[1][4] In short, all Danish residents are assigned a unique 10-digit personal identification number, the CPR number, upon birth or immigration. The CPR number serves as the key identifier in the nationwide registration of personal data, including contacts with the healthcare system. The CPR number also allows Statistics Denmark to produce updated population statistics at the individual level on a variety of different topics, including but not limited to demographics, income, education, and healthcare use.
The Danish healthcare system provides free healthcare to all residents at general practices and hospitals through a tax-paid system. This allows for long-term and virtually complete follow-up at the individual level across the different sources of healthcare data.
This review provides an overview of the two Danish healthcare research databases that collect routine individual-level biomarker data from general practitioners and hospital encounters: the regional Clinical Laboratory Information System Research (LABKA) Database at Aarhus University[5] and the nationwide Register of Laboratory Results for Research (RLRR).[6] These specific databases enable researchers to obtain very detailed and comprehensive biological information for research purposes.
Hospital laboratories are an integrated part of the public hospital system. Private medical laboratories play a minor role for routine biomarker analyses in Denmark, as they only provide a very limited number of the test results, and mainly for low throughput and highly specialized biomarkers, e.g., lactate dehydrogenase isoenzymes and metabolic intermediates.
Routine clinical biomarkers in the Danish healthcare system
Biomarkers are used in the everyday clinical workflow in general medical practices and in the hospital setting for diagnosing, screening, monitoring, and assessing prognoses of patients, as well as evaluating treatment effects and safety for a given patient. Upon physician request, biological samples (blood, urine, cerebrospinal fluid, and other body fluids) undergo biomarker analysis in public hospital laboratories, and thus biomarker data are recorded in the registries as a byproduct of healthcare provision. The biomarker results are registered in the electronic laboratory information systems (LISs) using the International System of Nomenclature, Properties, and Units (the NPU system).[7] Only a select few biomarker results are recorded by non-electronic methods, including some of the highly specialized biomarkers. The NPU system, an international standardised terminology for reporting on laboratory results, was established in 1960 by the International Union of Pure and Applied Chemistry (IUPAC) and the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC). The NPU system is equivalent to the Logical Observation Identifiers Names and Codes (LOINC) used in other parts of the world.[8] The organization of the NPU system complies with recommendations from these two leading international laboratory organizations. In Denmark, the NPU system was implemented in 2001, but some biomarkers do not comply with the NPU system and are coded using national or local codes. The results for these biomarkers are also included in the LISs.
The Danish hospital laboratories use a LIS for managing data on requisitions, specimen handling, transportation, and biomarker results. The LABKA database and the RLRR described in this review mainly cover routine biomarker results, including some results for therapeutic drug monitoring and genetic tests. Clinical microbiology and pathology are not included in these two research databases, but they are covered in other databases.[9][10][11]
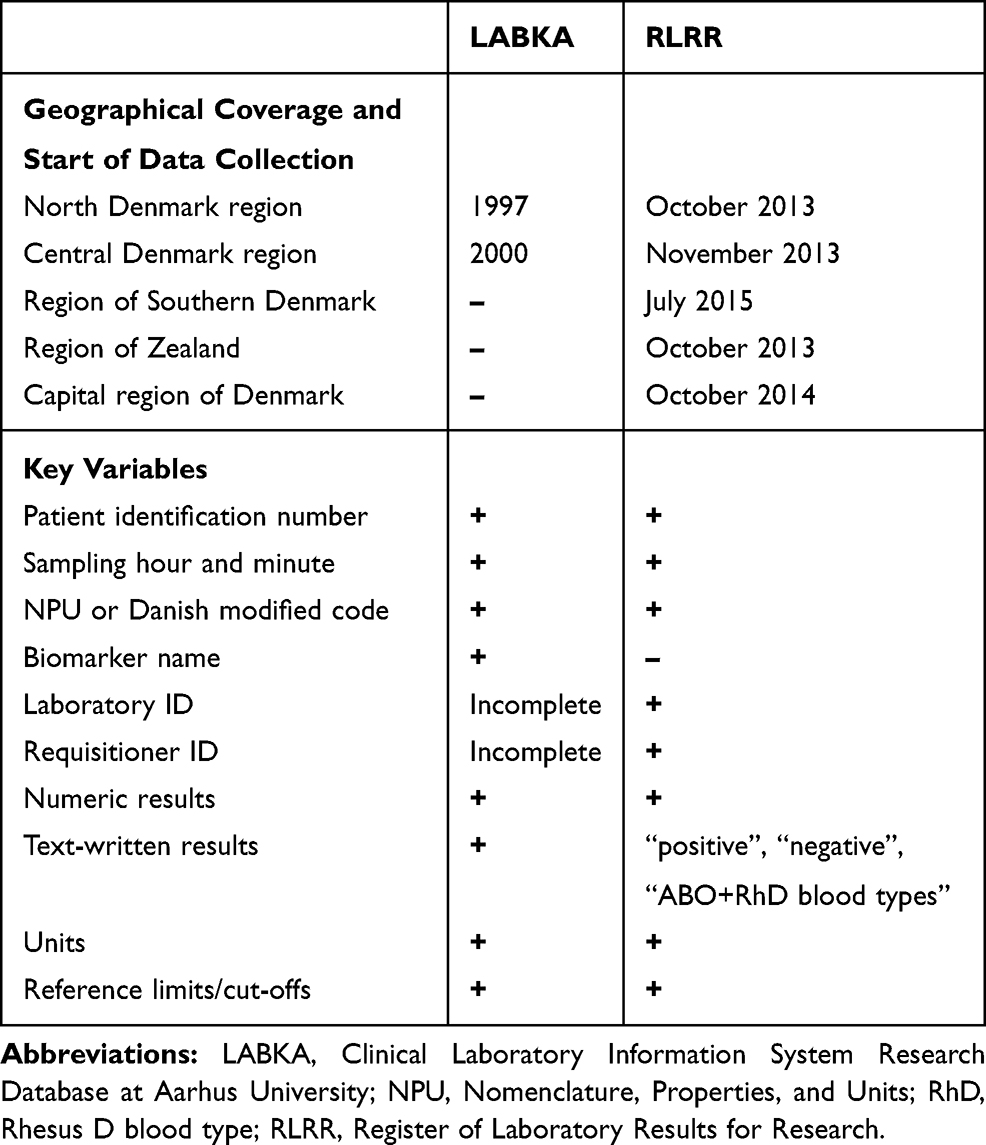
Specifications for the LABKA database and the RLRR are described in detail below and in Table 1. The two databases show some degree of overlap, since some geographical regions of Denmark are represented in both databases.
|
The LABKA database[5] is named after a specific LIS called LABKA. A previous publication has described the first version of the LIS as "a real-time computer system for handling and transfer of data to and from the hospital laboratory."[11] The LABKA database covers two (Northern and Central Danish Regions) of the five geographical regions in Denmark. These two regions currently have a combined population of 1.9 million inhabitants.[12] Data are considered complete for the geographical regions since 2005, but data from the late 1990s are available for some smaller geographical areas of the Northern and Central Danish Regions. The LABKA database holds biomarker results on more than 2.4 million individual patients dispersed over more than 6,000 different biomarker codes, coding for more than 1,700 different biomarkers. As an example, more than 8 million measurements of haemoglobin were performed on more than 1 million patients between 1999 and 2007. (Further details are found in an earlier publication.[5]) The LABKA database is hosted by the Department of Clinical Epidemiology, Aarhus University Hospital, Denmark.
The RLRR contains nationwide biomarker data from the Danish population of 5.8 million inhabitants.[13] The RLRR has varying temporal coverage as data collection started at different time points for the five Danish regions (Table 1). The database became available to researchers in 2018 and is hosted by the Danish Health Data Authority.[6]
Data collection
Content
The main variables contained in the two data sources are broadly comparable. They include the CPR number, date and time (hour and minute) of sampling, the NPU (or Danish modified) code or local code, identification codes of the laboratory and the requisitioner, the biomarker result, unit (e.g., mmol/L or ng/L), and lower and upper reference limits. The LABKA database also records the name of the biomarker and most text-written non-numeric results. The RLRR currently includes only the following text-written results: “positive,” “negative,” “ABO blood type,” and “rhesus blood type.” Hence, other text results are missing from the RLRR. The overall proportion of missing data has not been assessed, but the electronic data transfer should ensure a limited proportion of missing data.
Requisition of biomarkers through an electronic clinical user interface is essentially the same in hospitals, general practices, and private specialist clinics. Each requisition is transferred from the clinical user interface to the LIS. Most general practitioners handle sampling (e.g., venepuncture and urine or stool collection) and then send the samples by postal mail, courier services, or other transportation systems. At hospitals, laboratory technicians perform most venepunctures, and physicians or nursing staff collect other samples (e.g., urine, cerebrospinal fluid).
Point-of-care testing (POCT) equipment enables rapid bedside biomarker analysis results. POCT analyses are distinguished from analyses performed at hospital laboratories by separate NPU codes. Recording of POCT biomarker results in the databases requires online access to the LIS, which is inherent in most POCT equipment used in hospitals. However, results of POCT tests performed by general practitioners or specialist clinics are not recorded in the LIS.
The two laboratory databases are updated with different time intervals. The LABKA database is updated irregularly, at intervals of one to two years. The RLRR database is updated on a monthly basis from a national laboratory databank. This national databank transfers laboratory results both to a secured website for access by health professionals[14] and to a personal electronic medical file with unique personal access for individual Danish residents.[15]
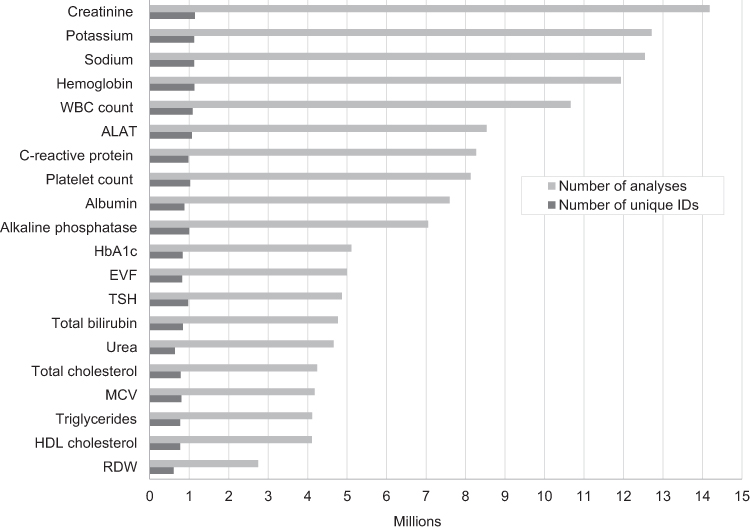
The pattern of test results follows clinical practice. Figure 1 provides an overview of the 20 most frequent biomarker analyses performed in the Central Denmark region from January 1, 2008 to December 31, 2018, including the total number of tests and the number of unique patients with at least one result for a given biomarker. As expected, the most commonly recorded results included basic haematological and infection tests, lipid and HbA1c levels, and measurements of liver, kidney, and thyroid function. The data we present from the LIS of Central Denmark is likely representative of Denmark as a whole, as Danish registries show a high degree of homogeneity for health care utilization across the five Danish regions.[16]
|
Data quality
The quality of biomarker results in the LIS databases is generally high. Most hospital laboratories in Denmark are accredited in accordance with the standards for medical laboratory testing specified by the International Organization for Standardization (ISO 15189).[17] As a result, quality management systems in Danish laboratories comply with international standards, including methodological and clinically relevant quality criteria such as detection limits, variation of analyses over time and across hospital laboratories, internal and external quality assurance, electronic transfer of test results to medical files and databases, procedures for handling errors, and systematic assessment of these quality standards. The accreditation status of an individual clinical laboratory can be found at the website of the Danish Accreditation Fund.[18]
Data resource use
Use of routine biomarker data in epidemiological research has tremendous potential, especially with linkage to other Danish healthcare registries. By using the CPR number, biomarker data can be linked with healthcare data at the individual level, such as hospital diagnosis, redeemed prescriptions, and causes of death. We refer to other publications for descriptions of available resources of Danish healthcare data.[1][2][3][4] Biomarker data provide detailed information about pathophysiological processes in individual patients and add significant value to the comprehensive network of Danish healthcare registries. In addition, the laboratory databases also allow identification of specific patients groups that are not readily captured by other data sources in Denmark[1], e.g., patients diagnosed and treated in general practice. Below, we provide some study examples, where biomarker data have been used. Since RLRR data only recently became available, the studies were based on data from the LABKA database.
Validation of registry data is fundamental to all types of epidemiological research. Biomarker data are a key resource for validating registry discharge diagnoses defined by biomarkers, such as anaemia, electrolyte disorders, lipid disorders, or diabetes.[19] One such study examined the sensitivity of hyponatraemia diagnoses in the Danish National Patient Registry (DNPR).[20] Only two percent of patients with a record of low sodium levels in the LABKA database had a hyponatraemia discharge diagnosis in the DNPR. The study thus revealed the incompleteness of hyponatraemia diagnoses in the DNPR. Laboratory data also can be used to evaluate measures of prevalence and incidence of diseases, risk factors for diseases, and the prognosis following abnormal laboratory test results among patients that are recorded with specific tests. As an example, a series of three studies examined the risk of elevated potassium levels, associated risk factors, and prognosis following hyperkalaemia in patients with diabetes, heart failure, and chronic kidney disease.[21][22][23] The uniqueness of these large population-based studies was their ability to separately appraise the risk of mild, moderate, and severe elevation of plasma potassium levels and to assess the risk of hyperkalaemia as a function of glycaemic control (HbA1c) and kidney function (eGFR). In another series of studies, the association between vitamin B12 levels and cancer was evaluated.[24][25][26] Not only were elevated vitamin B12 levels a marker of occult cancer, they was also associated with poor cancer prognosis and with the risk of venous thromboembolism among cancer patients. Finally, laboratory data can be used to assess the risk of specific drug side effects. A recent study found that the risk of hyponatraemia was higher among users of several different types of antidepressant drugs compared to non-users.[27]
Strengths and weaknesses
LABKA and the RLRR are valuable data resources for research. Their geographical and temporal completeness is relatively high, although the completeness varies between the data sources (Table 1). They provide population-based data encompassing most routine biomarker results from Danish hospital laboratories. Another strength of the databases stems from standardized quality assurance measures implemented in most Danish hospital laboratories. These standards ensure that erroneous test results caused by interferences—such as haemolysis in the blood tube, endogenous proteins in a patient’s blood, or prescribed medical drugs—are systematically detected and expunged so they are not provided to the clinician and not included in the databases. Unambiguous individual-level data linkage among the laboratory databases and other Danish healthcare registries ensures virtually endless opportunities for conducting epidemiological research.
Use of routine laboratory data for research purposes also has some potential limitations. Differences across laboratories in analytical methods and laboratory equipment imply that they do not necessarily produce comparable results and reference ranges for a given biomarker. Moreover, individual laboratories occasionally change their analytical methods, equipment, or units of measurement. Thus, biomarker levels and reference ranges may change over time within a given laboratory. However, the generally high number of observations makes it possible to account for such changes in most analyses. For example, analyses can be stratified by time period, or one can combine data from laboratories with comparable analytic methods and reference intervals. Another concern is that the indications for specific requested biomarkers and the reasons for repeated measurements are not readily available. It is beyond the scope of this article to assess regional differences or temporal changes in the pattern of biomarker results.
Comparison with other biomarker data sources
Other data sources that include biomarkers have been described in several publications.[28][29][30][31][32] They differ in several ways from the data sources described here. Some use the LISs to sample patients with results of specific markers, such as plasma creatinin[28][29], differential blood cell counts[30], or thyroid-stimulating hormone.[31] Hence, they are less comprehensive than the resources presented here. Others have used data directly from the LISs to assess research hypothesis.[32] This allows for more detailed information on, for example, specimen handling, but data directly from the LISs are limited to smaller geographical areas of Denmark.
Other data sources include biomarker results only from general practice, such as the U.K.-based General Practice Research Database[33] and The Health Improvement Network.[34]
Data resource access
Researchers interested in using data from the LABKA database could contact the Department of Clinical Epidemiology, Aarhus University Hospital, Denmark, regarding specific research projects.
The Danish Health Data Authority allows only Danish institutions to access its data, subsequent to approval of a formal application. The application must include the background and purpose of the study, and a description of the data sources and variables needed. Individual study data are available to researchers who successfully complete the application process, but they must access the data through servers behind firewalls. Transfer of individual-level data outside these servers is prohibited. Uploading of external data to the servers is possible. The Danish Health Data Authority ensures anonymization on their servers, and any access to non-anonymized data requires additional special approval. Access to registry data in Denmark for research purposes does not require approval from an ethics committee according to Danish law, but all studies should be approved by the Danish Data Protection Agency.[35] Foreign researchers can access data only through collaboration with a Danish institution that is approved for handling and accessing data on the servers of the Danish Health Data Authority. A fee for administration and data access is charged for projects that achieve approval with the Danish Health Data Authority.
Acknowledgements
We thank Pia Buys Petersen from the Danish Health Data Authority for her valuable input regarding the RLRR to the manuscript.
Author contributions
JFHA, ATH, HTS, and KAD conceived the idea for this manuscript. JFHA, ATH, and KAD drafted the initial manuscript. All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; gave final approval of the version to be published; and agree to be accountable for all aspects of the work.
Funding
JFHA has received a lecture fee on one occasion from Siemens Healthineers, Denmark, and a lecture on one occasion from Teva Denmark A/S within the last 36 months. The Department of Clinical Epidemiology, Aarhus University Hospital, receives funding for other studies from companies in the form of research grants to (and administered by) Aarhus University. None of these studies have any relation to the present study.
Disclosures and conflict of interest
Dr Johan Frederik Håkonsen Arendt has received a lecture fee on one occasion within the last 36 months from Siemens Healthineers, Denmark, and a lecture on one occasion from Teva Denmark A/S within the last 36 months. The lectures had no relation to the present study work. The Department of Clinical Epidemiology, Aarhus University Hospital, receives funding for other studies from companies in the form of research grants to (and administered by) Aarhus University. None of these studies have any relation to the present study. The sponsors of this study had no role in the initiation, planning, design or conduct of the study, data acquisition, management and analyses, interpretation of results, writing and approval of the manuscript, or the decision to submit the manuscript for publication. The researchers involved in this study declare their independence from the sponsors of the study. The authors report no other conflicts of interest in this work.
References
- ↑ 1.0 1.1 1.2 1.3 Schmidt, M.; Schmidt, S.A.J.; Adelborg, K. et al. (2019). "The Danish health care system and epidemiological research: From health care contacts to database records". Clinical Epidemiology 11: 563–91. doi:10.2147/CLEP.S179083. PMC PMC6634267. PMID 31372058. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6634267.
- ↑ 2.0 2.1 Thygesen, L.C.; Ersbøll, A.K. (2011). "Danish population-based registers for public health and health-related welfare research: introduction to the supplement". Scandinavian Journal of Public Health 39 (7 Suppl.): 8–10. doi:10.1177/1403494811409654. PMID 21775344.
- ↑ 3.0 3.1 Sørensen, H.T.; Pedersen, L.; Jørgensen, J. et al. (2016). "Danish clinical quality databases - an important and untapped resource for clinical research". Clinical Epidemiology 8: 425-427. doi:10.2147/CLEP.S113265. PMID 27843338.
- ↑ 4.0 4.1 Schmidt, M.; Pedersen, L.; Sørensen, H.T. (2014). "The Danish Civil Registration System as a tool in epidemiology". European Journal of Epidemiology 29 (8): 541–9. doi:10.1007/s10654-014-9930-3. PMID 24965263.
- ↑ 5.0 5.1 5.2 Grann, A.F.; Erichsen, R.; Nielsen, A.G. et al. (2011). "Existing data sources for clinical epidemiology: The clinical laboratory information system (LABKA) research database at Aarhus University, Denmark". Clinical Epidemiology 3: 133-8. doi:10.2147/CLEP.S17901. PMID 21487452.
- ↑ 6.0 6.1 "Laboratoriedatabasen". Sundhedsdata-Styrelsen. 2018. https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/doedsaarsager-og-biologisk-materiale/laboratoriedatabasen. Retrieved 12 March 2018.
- ↑ C-SC-NPU of the IFCC and UIPAC et al. (2009). "Clinical laboratory sciences data transmission: the NPU coding system". Studies in Helath Technology and Informatics 150: 265–9. PMID 19745311.
- ↑ Forrey, A.W.; McDonald, C.J.; DeMoor, G. et al. (1996). "Logical observation identifier names and codes (LOINC) database: A public use set of codes and names for electronic reporting of clinical laboratory test results". Clinical Chemistry 42 (1): 81–90. doi:10.1093/clinchem/42.1.81. PMID 8565239.
- ↑ Gradel, K.O.; Schønheyder, H.C.; Arpi, M. et al. (2014). "The Danish Collaborative Bacteraemia Network (DACOBAN) database". Clinical Epidemiology 6: 301–8. doi:10.2147/CLEP.S66998. PMC PMC4172047. PMID 25258557. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4172047.
- ↑ Schønheyder, H.C.; Søgaard, M. (2010). "Existing data sources for clinical epidemiology: The North Denmark Bacteremia Research Database". Clinical Epidemiology 2: 171-8. doi:10.2147/clep.s10139. PMC PMC2943179. PMID 20865114. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2943179.
- ↑ 11.0 11.1 Christiansen, J.U.; Maruard, C.D.; Nielsen, H.C. (1989). "LABKA. A real-time computer system for the clinical laboratory". Scandinavian Journal of Clinical and Laboratory Investigation Supplementum 194: 57–61. PMID 2772556.
- ↑ Erichsen, R.; Lash, T.L.; Hamilton-Dutoit, S.J. et al. (2010). "Existing data sources for clinical epidemiology: The Danish National Pathology Registry and Data Bank". Clinical Epidemiology 2: 51-6. doi:10.2147/clep.s9908. PMC PMC2943174. PMID 20865103. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2943174.
- ↑ "Folketal". Danmarks Statistik. 2019. https://www.dst.dk/da/Statistik/emner/befolkning-og-valg/befolkning-og-befolkningsfremskrivning/folketal. Retrieved 16 October 2019.
- ↑ "Laboratoriesvarportalen". Medcom. 2019. https://www.medcom.dk/opslag/support/laboratoriesvarportalen. Retrieved 16 October 2019.
- ↑ "Din sundhedsportal". Sundhed. 2019. https://www.sundhed.dk/. Retrieved 16 October 2019.
- ↑ Henriksen, D.P.; Rasmussen, L.; Hansen, M.R. et al. (2015). "Comparison of the Five Danish Regions Regarding Demographic Characteristics, Healthcare Utilization, and Medication Use--A Descriptive Cross-Sectional Study". PLoS One 10 (10): e0140197. doi:10.1371/journal.pone.0140197. PMC PMC4595085. PMID 26439627. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4595085.
- ↑ "ISO 15189:2012 Medical laboratories — Requirements for quality and competence". International Organization for Standardization. November 2012. https://www.iso.org/standard/56115.html. Retrieved 16 October 2019.
- ↑ "Search for Accredited Companies". The Danish Accreditation Fund. http://english.danak.dk/database-of-accredited-companies.
- ↑ Schmidt, M.; Schmidt, S.A.J.; Sandegaard, J.L. et al. (2015). "The Danish National Patient Registry: A review of content, data quality, and research potential". Clinical Epidemiology 7: 449–90. doi:10.2147/CLEP.S91125. PMC PMC4655913. PMID 26604824. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4655913.
- ↑ Holland-Bill, L.; Christiansen, C.F.; Ulrichsen, S.P. et al. (2014). "Validity of the International Classification of Diseases, 10th revision discharge diagnosis codes for hyponatraemia in the Danish National Registry of Patients". BMJ Open 4 (4): e004956. doi:10.1136/bmjopen-2014-004956. PMC PMC4010845. PMID 24760354. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4010845.
- ↑ Thomsen, R.W.; Nicolaisen, S.K.; Hasvold, P. et al. (2018). "Elevated Potassium Levels in Patients With Congestive Heart Failure: Occurrence, Risk Factors, and Clinical Outcomes: A Danish Population-Based Cohort Study". Journal of the American Heart Association 7 (11): e008912. doi:10.1161/JAHA.118.008912. PMC PMC6015368. PMID 29789332. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6015368.
- ↑ Thomsen, R.W.; Nicolaisen, S.K.; Adelborg, K. et al. (2018). "Hyperkalaemia in people with diabetes: Occurrence, risk factors and outcomes in a Danish population-based cohort study". Diabetic Medicine 35 (8): 1051-1060. doi:10.1111/dme.13687. PMID 29790603.
- ↑ Thomsen, R.W.; Nicolaisen, S.K.; Hasvold, P. et al. (2018). "Elevated potassium levels in patients with chronic kidney disease: occurrence, risk factors and clinical outcomes-a Danish population-based cohort study". Nephrology, Dialysis, Transplantation 33 (9): 1610-1620. doi:10.1093/ndt/gfx312. PMID 29177463.
- ↑ Arendt, J.F.H.; Farkas, D.K.; Pedersen, L. et al. (2016). "Elevated plasma vitamin B12 levels and cancer prognosis: A population-based cohort study". Cancer Epidemiology 40: 158–65. doi:10.1016/j.canep.2015.12.007. PMID 26724465.
- ↑ Arendt, J.F.H.; Farkas, D.K.; Pedersen, L. et al. (2017). "Elevated plasma vitamin B12 levels and risk of venous thromboembolism among cancer patients: A population-based cohort study". Thrombosis Research 156: 177-183. doi:10.1016/j.thromres.2017.06.022. PMID 28667844.
- ↑ Arendt, J.F.H.; Pedersen, L.; Nexo, E. et al. (2013). "Elevated plasma vitamin B12 levels as a marker for cancer: A population-based cohort study". Journal of the National Cancer Institute 105 (23): 1799–805. doi:10.1093/jnci/djt315. PMC PMC3848986. PMID 24249744. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3848986.
- ↑ Leth-Møller, K.B.; Hansen, A.H.; Torstensson, M. et al. (2016). "Antidepressants and the risk of hyponatremia: A Danish register-based population study". BMJ Open 6 (5): e011200. doi:10.1136/bmjopen-2016-011200. PMC PMC4874104. PMID 27194321. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4874104.
- ↑ 28.0 28.1 Runesson, B.; Gasparini, A.; Qureshi, A.R. et al. (2016). "The Stockholm CREAtinine Measurements (SCREAM) project: Protocol overview and regional representativeness". Clinical Kidney Journal 9 (1): 119-27. doi:10.1093/ckj/sfv117. PMC PMC4720196. PMID 26798472. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4720196.
- ↑ 29.0 29.1 Henriksen, D.P.; Dankier, P.; Hallas, J. et al. (2019). "Sixteen years of creatinine measurements among 460 000 individuals-The Funen Laboratory Cohort (FLaC), a population-based pharmacoepidemiological resource to study drug-induced kidney disease". Basic and Clinical Pharmacology and Toxicology 124 (5): 582-590. doi:10.1111/bcpt.13167. PMID 30417606.
- ↑ 30.0 30.1 Anderen, C.L.; Siersma, V.D.; Karlslund, W. et al. (2014). "The Copenhagen Primary Care Differential Count (CopDiff) database". Clinical Epidemiology 6: 199-211. doi:10.2147/CLEP.S60991. PMC PMC4062550. PMID 24966694. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4062550.
- ↑ 31.0 31.1 Laulund, A.S.; Nybo, M.; Brix, T.H. et al. (2014). "Duration of thyroid dysfunction correlates with all-cause mortality. The OPENTHYRO Register Cohort". PLoS One 9 (10): e110437. doi:10.1371/journal.pone.0110437. PMC PMC4207745. PMID 25340819. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4207745.
- ↑ 32.0 32.1 Hansen, A.T.; Hoffmann-Lücke, E.; Nielsen, B.K. et al. (2017). "Delayed sample arrival at the laboratory does not lead to more false negatives in the Danish population screening for colorectal cancer". Scandinavian Journal of Clinical and Laboratory Investigation 77 (8): 685-688. doi:10.1080/00365513.2017.1379091. PMID 28933963.
- ↑ Williams, T.; van Staa, T.; Puri, S. et al. (2012). "Recent advances in the utility and use of the General Practice Research Database as an example of a UK Primary Care Data resource". Therapeutic Advances in Drug Safety 3 (2): 89-99. doi:10.1177/2042098611435911. PMC PMC4110844. PMID 25083228. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4110844.
- ↑ Blak, B.T.; Thompson, M.; Dattani, H. et al. (2011). "Generalisability of The Health Improvement Network (THIN) database: Demographics, chronic disease prevalence and mortality rates". Informatics in Primary Care 19 (4): 251-5. doi:10.14236/jhi.v19i4.820. PMID 22828580.
- ↑ Ludvigsson, J.F.; Håberg, S.E.; Knudsen, G.P. et al. (2015). "Ethical aspects of registry-based research in the Nordic countries". Clinical Epidemiology 7: 491–508. doi:10.2147/CLEP.S90589. PMC PMC4664438. PMID 26648756. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4664438.
Notes
This presentation is faithful to the original, with only a few minor changes to presentation, grammar, and spelling. In some cases important information was missing from the references, and that information was added. The original URL to the Danish search for accredited companies is broken; it has been replaced with a working URL for this version.