Users’ perspectives on a picture archiving and communication system (PACS): An in-depth study in a teaching hospital in Kuwait
| Full article title | Users’ perspectives on a picture archiving and communication system (PACS): An in-depth study in a teaching hospital in Kuwait |
|---|---|
| Journal | JMIR Medical Informatics |
| Author(s) | Buabbas, Ali Jassem; Al-Shamali, Dawood Ameer; Sharma, Prem; Haidar, Salwa; Al-Shawaf, Hamza |
| Author affiliation(s) | Kuwait University, Mubarak AlKabeer Hospital |
| Primary contact | Email: ali.buabbas [at] hsc.edu.kw; Phone: 965 25319504 |
| Editors | Eysenbach, G. |
| Year published | 2016 |
| Volume and issue | 4 (2) |
| Page(s) | e21 |
| DOI | 10.2196/medinform.5703 |
| ISSN | 2291-9694 |
| Distribution license | Creative Commons Attribution 2.0 |
| Website | http://medinform.jmir.org/2016/2/e21/ |
| Download | http://medinform.jmir.org/2016/2/e21/pdf (PDF) |
Abstract
Background: The picture archiving and communication system (PACS) is a well-known imaging informatics application in health care organizations, specifically designed for the radiology department. Health care providers have exhibited willingness toward evaluating PACS in hospitals to ascertain the critical success and failure of the technology, considering that evaluation is a basic requirement.
Objective: This study aimed to evaluate the success of a PACS in a regional teaching hospital of Kuwait, from users’ perspectives, using information systems success criteria.
Methods: An in-depth study was conducted by using quantitative and qualitative methods. This mixed-method study was based on: (1) questionnaires, distributed to all radiologists and technologists and (2) interviews, conducted with PACS administrators.
Results: In all, 60 questionnaires were received from the respondents. These included 39 radiologists (75% response rate) and 21 technologists (62% response rate), with the results showing almost three-quarters (74%, 44 of 59) of the respondents rating PACS positively and as user-friendly. This study’s findings revealed that the demographic data, including computer experience, was an insignificant factor, having no influence on the users’ responses. The findings were further substantiated by the administrators’ interview responses, which supported the benefits of PACS, indicating the need for developing a unified policy aimed at streamlining and improving the departmental workflow.
Conclusions: The PACS had a positive and productive impact on the radiologists’ and technologists’ work performance. They were endeavoring to resolve current problems while keeping abreast of advances in PACS technology, including teleradiology and the mobile image viewer, which is steadily increasing in usage in the Kuwaiti health system.
Keywords: PACS evaluation, user perspective, IS success, imaging informatics, radiology
Introduction
The picture archiving and communication system (PACS) is a well-known imaging informatics application in health care organizations, specifically designed for the radiology department. A PACS could be defined as “an electronic information system (IS) used to acquire, store, transmit, and display medical images.”[1] Using a PACS in a hospital has innumerable benefits at various levels.[2] At the management level, this technology has direct implications for cost reduction, rendering the film production process redundant. At the departmental level, the technology enhances productivity, as all tasks are performed digitally and swiftly. And at the clinical level, image interpretation and diagnosis become more precise and accurate.[3] For these reasons, health care organizations are increasingly adopting the PACS in their clinical radiology departments, despite the high costs, to benefit from the full advantages of using the technology. PACSs are currently being applied in many medical imaging projects around the world, such as in the United States, the United Kingdom, and Asia. However, the available literature reveals gaps with regard to the systems’ effectiveness and efficiency concerning their intended use.
The existing literature abounds with studies evaluating the PACS.[4] However, these evaluations invariably had different focuses and objectives; for instance, there are studies on the PACS before and after the system’s implementation[5], users’ satisfaction[6], PACS acceptance[7], cost-effectiveness[8][9], and the system’s efficiency concerning its use and in saving time.[10] The most widely used form of the PACS evaluation concerns its impact on users.[4][11][12]
In PACS research and practice, once the system has been adopted and implemented, it becomes imperative to evaluate the technology’s effectiveness within an organization.[13] For all practical purposes, evaluation could be defined as “the process of describing the implementation of an information resource and judging its merits and worth.”[14] IS deployment may invariably lead to unintended consequences, affecting the chances of the technology’s success.[14] Several researchers have, therefore, recommended evaluation studies specially focused on PACSs to assess their impact in clinical practice [4,15].[4][15]
It is of paramount significance to investigate the success of the PACS, exploring the factors responsible for the success or failure to determine its worth clinically, based on the direct users of this system.
The conceptual basis of this study is focused on this: the impact of a PACS in a regional hospital in Kuwait based on specific criteria. This study is the first of its kind in Kuwait, there being a scarcity of literature in this field.
Research questions
The research questions were specifically as follows: (1) What impact does the PACS have on the clinical practice of radiologists and technologists in the radiology department of Mubarak Al-Kabeer Hospital? (2) Has the use of the PACS proven successful in improving the radiology department’s work performance?
This study aimed at evaluating the success of the PACS in clinical practice, in a bid to determine the technology’s merits for radiologists and technologists, including its drawbacks.
Methods
Research settings
The universe of this study was Mubarak Al-Kabeer Teaching Hospital, which is one of the five regional hospitals in the State of Kuwait. Table 1 presents the site’s profile.
| ||||||||||||||||||
This general hospital is a university-teaching hospital in Kuwait and was chosen because it is always at the forefront of development and advanced medicine. Therefore, to ensure the full advantage of the health information system (HIS), the PACS’s success needed to be verified. The PACS was first introduced in the radiology department of Mubarak Al-Kabeer Hospital in 2004, marking the transition of clinical services from a film-based system to an electronic-based system. The PACS used is an off-the-shelf, Oracle-based HIS (GE Centrisity RIS i 4.2 plus, GE PACS IW 3.7.3.9 SP 3). The PACS currently has 35 workstations, with a server capacity of 64 terabytes. Radiologists use the PACS to view images through the radiology information system (RIS), which they use to report their cases. The reports generated by the RIS are then sent to the PACS, through which final reports can be sent to the HIS. The treating physician needs to submit an access request to see patients’ images on the PACS. In June 2013, the PACS software was upgraded, and currently the system is fully integrated technically with the RIS and the HIS, providing the users with a secure system.
Study design
An in-depth study was conducted by using quantitative and qualitative methods. This mixed-method study was based on: (1) survey questionnaires, which were distributed to gather information from radiologists and technologists in the radiology department of Mubarak Al-Kabeer Hospital and (2) semi structured interviews, which were conducted to gather empirical information from the PACS administrators. Ethical approval for the study was obtained from the research department of the Ministry of Health, Kuwait.
To gather the responses of radiologists and technologists concerning the use of the PACS in their clinical practice, a validated questionnaire from a previous study was used.[16] The questionnaire was translated from French into English through an official translation office in Kuwait. The English version of the questionnaire was pretested with five radiologists and three technologists to ensure the suitability and usability of the questions. Accordingly, a number of amendments were made to the questionnaire. These included excluding questions that were found to be irrelevant to the technologists’ use of the PACS, which comprised items that focused on retrieving, displaying, comparing, and manipulating images, including confidence level. In addition, a seven-point Likert scale was changed to five points to make it easier and more familiar for the respondents.
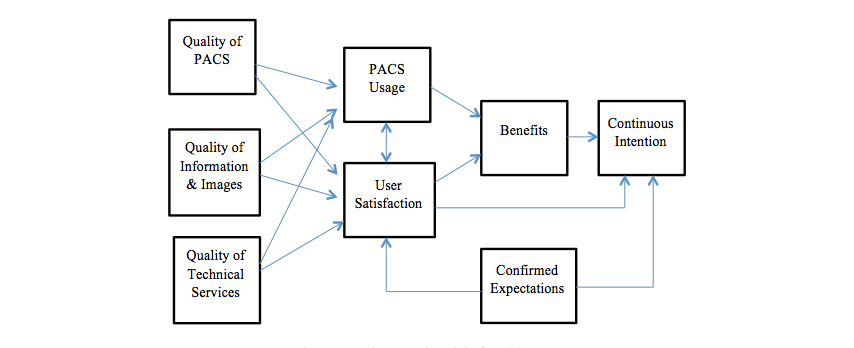
In this study, evaluating the PACS’s success was based on an integrated multidimensional model, which was constructed from the model primarily developed by DeLone and McLean[17][18], later developed with two constructs added to the model, namely system continuance intention and confirmation of expectations.[16] (See Figure 1.)
|
The questionnaire comprised seven sections (Textbox 1) for assessing the users’ perspectives on eight interrelated dimensions of the PACS success model. These included: (1) perceived system quality; (2) perceived information quality; (3) perceived service quality; (4) system usage; (5) user satisfaction; (6) perceived net benefits; (7) system continuance intention; and (8) confirmed expectations. The questionnaire was distributed to all radiologists and radiology technologists who had used the PACS in their clinical practice for the last two years.
|
The data gathered through the questionnaire were complemented by conducting semi-structured interviews with PACS administrators to gain an understanding of the prevailing clinical environment, which entails them communicating with radiologists, doctors, and technologists, including providing information technology services and support.[19] Their experience further enriched the information gathered and the study’s purpose.
The focus of the interviews was primarily similar to that of the questionnaire: to gain a deeper insight into the response patterns of the respondents. The interviews were conducted with the radiology technologists, who are responsible for administering the PACS and overseeing the RIS operations in the radiology department.
Statistical analysis
Data management, analysis, and graphical presentation were carried out using the software Statistical Package for the Social Sciences (SPSS), version 22.0. The questionnaire was evaluated for internal consistency and reliability, and Cronbach alpha values were estimated for major perspectives by combining the Likert scale items for specific aspects, including quality, information, images, technical support and usage, user satisfaction, and overall opinion on the PACS. The descriptive statistics analysis generated frequencies and percentages for all the five-point Likert scale items (1 as lowest or strongly disagree and 5 as highest or strongly agree) in the questionnaire. The Likert scale data were also analyzed to find average values for overall responses and to compare the mean (±standard deviation, SD) between radiologists and technologists using t tests or nonparametric Mann-Whitney tests. The quantitative or continuous variables, age, duration of use (h), and minutes saved every day were first ascertained for normal distribution, applying the Kolmogorov-Smirnov test and were presented as mean ± SD and range for normally distributed variables and as median, range and interquartile (IQ) for skewed data. The chi-square or Fisher exact test was applied to find any association or significant difference between categorical variables. The Spearman correlation coefficient (rho) was used to find any correlations among the number of hours worked, the use of the PACS, and the minutes saved in daily practice. The two-tailed probability value P<.05 was considered statistically significant.
Results
Questionnaires
Respondent demographics
The study’s overall response rate was 70%: 75% of the radiologists and 62% of the technologists of the radiology department. The study had 60 respondents: 39 radiologists (mean age = 36±7.5 SD) and 21 technologists (mean age = 28±10 SD). The respondents’ ages varied between 20 and 60 years, with the majority (85%; 51 of 60) aged younger than 40 years. The respondents’ average self-rated level of familiarity with computers was 4.8 ± 1.34 (mean ± SD) on a scale of 1-7, and 41% (24 of 59) of the respondents had earlier experience with PACSs before working at this radiology department.
Evaluation of Different Perspectives on the PACS
The overall responses on different perspectives were analyzed, and composite reliability and coefficients (Cronbach alpha) were computed and presented in Table 2, along with mean and range for each perspective. The Cronbach alpha values ranged between .73 and .96, except for one as shown in in Table 2. System quality, images produced, and services all had high (>.9) Cronbach alpha values.
The overall perspectives of users have been presented on the following aspects:
System quality
Almost three-quarters (75%; 44 of 59) of the respondents rated the PACS positively and as user-friendly, with a mean of 3.28 (Table 2). Comparatively fewer (64%; 38 of 59) respondents mentioned some drawbacks of the system, such as it being temporarily out-of-service or not working, having numerous bugs, causing wait times at the workstations, and exhibiting reduced screen quality which slowed down PACS use. The majority (81%; 48 of 59) agreed that the PACS had improved the quality of services at the radiology department (mean=4.01). However, some suggestions were provided by respondents (mean=3.57) with regard to the system’s improvement, including the provision of more options and investment in upgrading the visualization equipment (PC monitors).
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Information quality
In all, 90% (53 of 59) agreed that the PACS produced better and higher-quality information (mean=3.75) that was accurate, updated, relevant, and timely. The system also provided complete patient information, including adequate access to patients’ historical data (mean=3.56).
Image quality
The PACS users were extremely satisfied with regard to the quality of the images produced, ease of understanding, and relevance (mean=4.27). They found that the PACS produced much better images compared to traditional film (mean=4.33).
Technical support and services
The PACS users were quite satisfied with technical support (mean=3.60) and the reliability, promptness, and dependability of services.
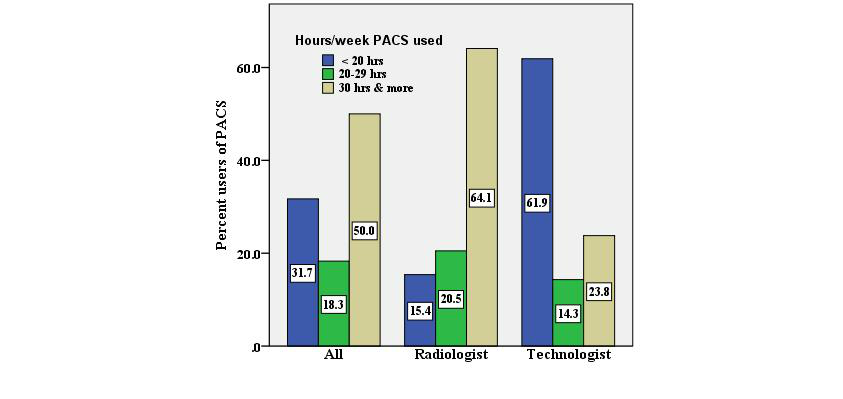
Use of PACS and satisfaction
In all, 50% (30 of 60) of the respondents mentioned using the PACS for more than 30 hours per week (Figure 2), although a significant difference was found regarding the duration of PACS use (hours/week) between radiologists and technologists (P<.001). A high level of user satisfaction was shown with regard to their experience in using the PACS (mean=3.65). The usage of various tools, including changing display format, retrieving, and “split screening” to compare images, was found to be quite satisfactory (mean=3.57), especially among radiologists.
|
Future use and expectations on PACS
In all, 83.9% (mean=3.39) of PACS users mentioned their expectations better than what they expected originally and showed intention to continue using PACS.
Overall opinions and impact of PACS
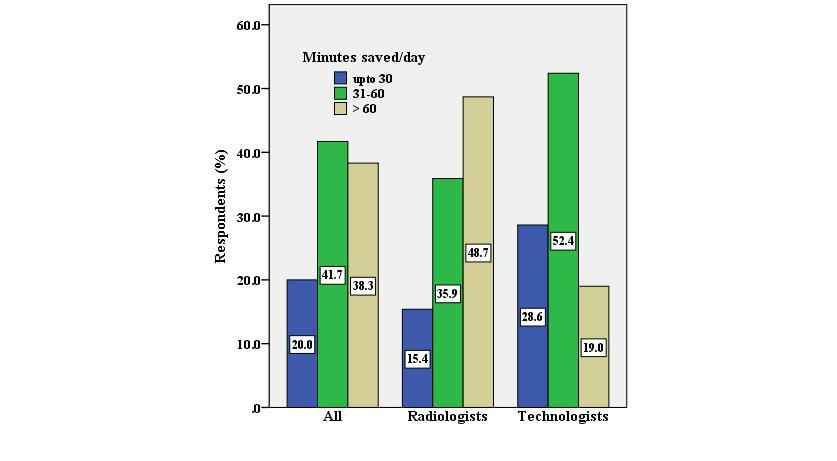
Based on 21 different statements, 93% (56 of 60) of the PACS users showed consensus on various aspects of the system’s benefits and effectiveness (mean=4.01), and the mean was significantly higher for technologists as compared with radiologists (4.22 vs 3.89). Furthermore, the results showed that 80% (48 of 60) of the PACS users reported saving more than 30 minutes of their practice time each day, whereas 38% (23 of 60) mentioned saving more than an hour each day.
Radiologists versus technologists
Table 3 summarizes the comparison between radiologists’ and technologists’ responses with regard to their perspectives concerning the PACS. The mean values were significantly higher for the technologists as compared with the radiologists, especially concerning quality, information, patient data, technical support, and overall opinion on impact of the PACS (P<.05). Both professionals showed the highest level of satisfaction (mean >4) with regard to image produced, and their overall opinions on PACS demonstrated improved quality and services (radiologist 3.9 and technologists 4.2).
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
In total, 49% (19 of 39) of the radiologists mentioned saving more than 60 minutes every day, as compared to 19% (4 of 21) of the technologists (P=.048) (Figure 3).
|
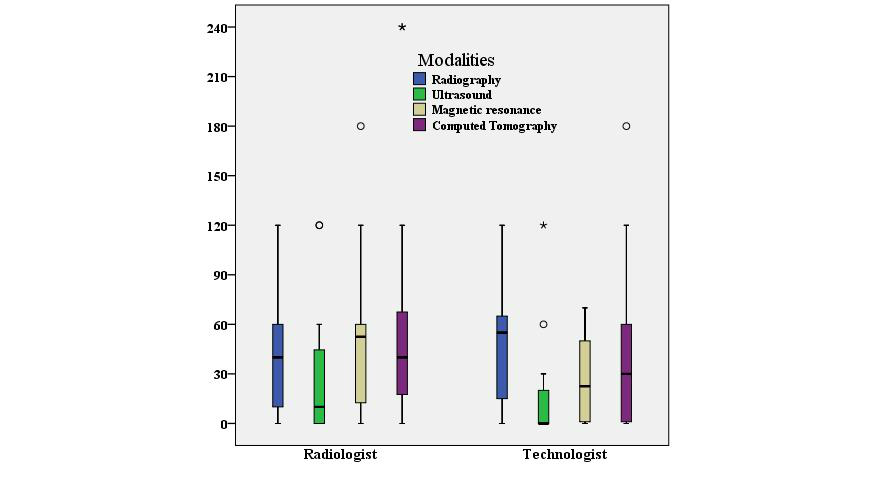
During use of the PACS, both professional groups reported significant savings in the working time for different modalities, though with much variation (the Kolmogorov–Smirnov tests showed a skewed distribution); the median and interquartile have been presented in Figure 4 as a box-plot. The maximum number of minutes saved was 52 minutes (median time) by radiologists in magnetic resonance imaging and 50 minutes by technologists in radiography.
|
A significant positive correlation was observed between the number of hours using the PACS and the minutes saved in daily practice since the introduction of the PACS (r=0.27, P=.037).
The level of prior familiarity with computers was found to be similar between the radiologists (4.84±1.34 SD) and the technologists (4.71±1.35 SD) and did not make any significant difference either in the average duration (hours/week) of working with the PACS or the time saved (minutes/day) during practice.
The results of the open-ended questions showed that 24% (9 of 38) of the radiologists and 33% (7 of 21) of the technologists stated that storing, retrieving, and comparing images were the most positive elements associated with the use of the PACS. By contrast, 33% (13 of 39) of the radiologists and 43% (9 of 21) of the technologists stated that frequent glitches were the most negative element associated with the PACS.
Overall, the study’s findings revealed that both the radiologists and the technologists perceived the adoption of the PACS positively. The mean scores were mostly above 3 or 4 on a scale of 1-5. The mean scores for image quality and information produced were 4.3 and 3.8, respectively. The users seemed quite satisfied with the services and technical support, with a mean score of 3.6 and showed satisfaction in working with the PACS (mean=3.65). The PACS users clearly mentioned improved services and quality since the system came into practice, with a mean score of 4.
Interviews
The opinions of the PACS administrators were obtained by using the interview method, for which a series of semi-structured questions on specific themes (Textbox 1) provided the basis for soliciting information.
At the time of the interviews, Mubarak Al-Kabeer Hospital had five PACS administrators. For scheduling the interviews, requisite permission was taken from the head of the radiology department, and interview sessions were arranged with the staff during their respective work breaks, over a five-day period. Each interview session lasted approximately 50 minutes. The interviews were transcribed, and the responses were coded and analyzed using thematic analysis.
The interview results showed that all the interviewees had a BSc degree in radiological sciences, with their ages ranging between 25 and 35 years, and each having work experience of 2-5 years in PACS administration. Of the interviewees, only three had undertaken an introductory training program abroad on PACS use and management.
Perceived system quality
The interview responses confirmed that the PACS provided easy access to authorized users, each with a user identification (ID) number and password, thereby providing a secured workspace depending on the user’s position. For instance, a radiology technologist’s access is limited to only viewing the reporting screen, with no authorization to change or manipulate it, thus preserving the data, with no hacking or security problems ever encountered or reported.
The interviewees unanimously agreed that the PACS was user friendly and hassle free in its functionality. In one of the interviewee’s words, “We haven’t experienced any complaints from radiologists regarding the clarity of the PACS’s features, or any difficulties in moving between its functions,” further adding that training in the PACS should be a prerequisite before its use.
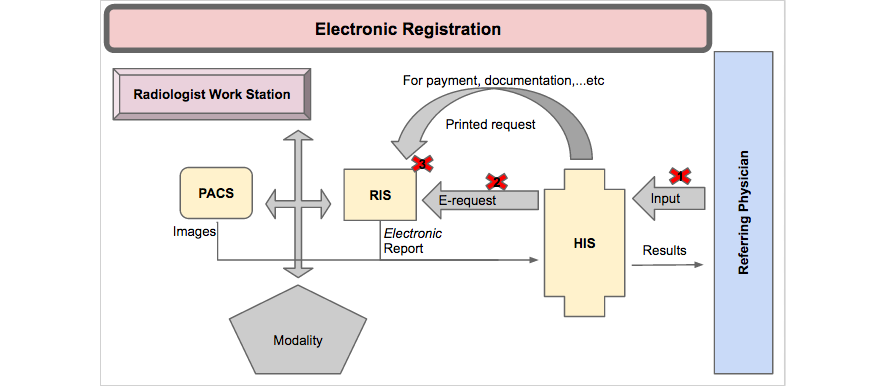
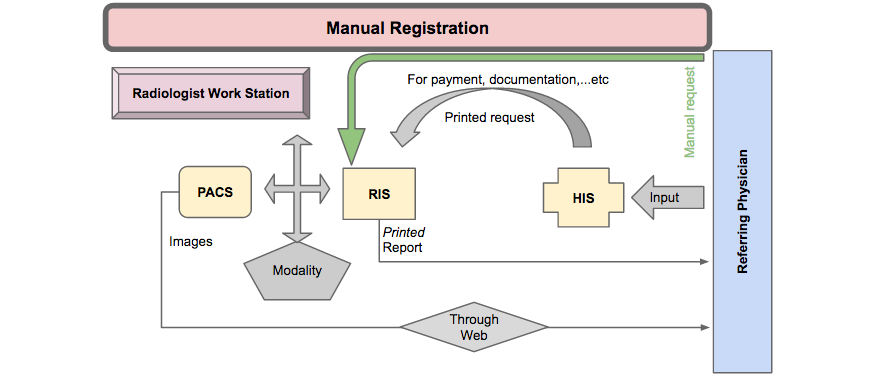
The participants also endorsed the reliability and consistency of the existing hardware, including computer systems, networks, and printers, with the software used. The interviews further revealed that the PACS was fully integrated and compatible with the RIS and the HIS, although the workflow did not follow the planned process, as Figure 5 demonstrates. According to one interviewee, “The real mistakes are not coming from the PACS but from humans, so they’re human errors.” The interview responses also highlighted that the problems associated with PACS integration and compatibility with the RIS and the HIS were the result of disorganized workflow, as shown in Figure 5.
|
Figure 5 (above) illustrates the workstations where electronic registration of patients through the HIS and the RIS failed due to receptionist errors such as: (1) no data entry into HIS, manual registration in the RIS; (2) failure of communication between the HIS and the RIS, manual registration in the RIS; (3) and incorrect registration at reception, manual registration in the RIS (Figure 6).
|
The manual registration at these three workstations resulted in: (1) a lack of direct access to patients’ imaging results through the HIS; (2) the creation of multiple PACS numbers for the same patient, making it difficult to retrieve previous reports for comparison, as well as the loss of patient data; and (3) delayed patient case management due to a failure in the rapid delivery of results.
Perceived information quality
The interviewees agreed that the PACS provided a standard format for the acquisition of accurate and complete information, together with images, concerning the patients’ medical cases, including their name, age, gender, national identification number, medical record number, and medical history. The lapses that occurred in the recorded information were attributed to the registration staff of the diagnostic radiology department because of their noncompliance to instructions, which resulted in incomplete data records of patients at the time of registration.
Perceived image quality
The interview responses indicated that one of the main roles of PACS administrators was to ensure that the images were transferred and displayed with clarity to facilitate studying and reporting. The participants further confirmed that “We experience hangs in the images in PACS, but at an acceptable rate” and no complaints were mentioned concerning image manipulation and management.
Perceived technical support services
As the interviewees mentioned, the main IT support is delivered through the company that sold the PACS. This usually happens when the PACS administrators face a technical problem that can only be solved through the main IT support at the company. Thus, the PACS administrators asked to have some power to authorize them to solve the technical issues within the radiology department. One of the interviewees stated: “…even when we want to connect a new printer to the PACS, we have to call the main IT support to perform this function for us.” However, all of the interviewees complimented the IT support services at the company for their prompt responses to any technical issues.
Impact of PACS on clinical practice
PACS has an impact on the clinical practice of radiologists and technologists, as shown in the interviews' results.
Perceived net benefits of the PACS
From the interviews, it was easy to see that the PACS has increased users’ productivity in comparison to the traditional filming system by minimizing their effort and time. In addition, the retaking of images is not required, as the PACS facilitates image storage and retrieval faster and over a longer period. “We are happy with the PACS’s benefits,” reported one interviewee, although the system has slowed in speed due to the huge number of cases, with the intervening procedures passing through several modalities, such as computed tomography and magnetic resonance imaging. There is also the possibility of missed images, especially concerning unknown IDs, although these could be traced using the patient’s civil ID, the patient’s PACS ID, or the excision ID of images.
User satisfaction with the PACS
All the interviewees were apparently satisfied with the PACS; however, the technology-associated problems need to be addressed to optimize the system’s versatility and performance.
Opinions on the PACS
Overall, from the interviews, the responses revealed that as long as the image is electronically collected, stored, and communicated to another system successfully, the productively of work will be increased, diagnosis will be precisely performed, the patient will be treated accurately and quickly, and health services will be improved.
Expectations of the current PACS and future trends
The interviewees expressed satisfaction in using the PACS system but also highlighted the need for resolving the current problems, as well as to keep abreast of the latest advances in PACS operations, to meet the growing demands of the Kuwaiti health system. The emerging requirements for potential trends in the future concern the areas of: (1) teleradiology services (for radiologists to use the PACS anywhere and anytime); (2) a mobile image viewer for faster accessibility to images; (3) speech recognition functions; (4) computer-assisted diagnosis (CAD); (5) advanced training; and (6) recruiting health informatics graduates to support the PACS administrators.
Discussion
In general, the study’s findings revealed that the PACS has had a productive impact on the staff’s clinical practice. Despite some of the technical limitations of the infrastructure, most of the respondents rated the system positively and as user-friendly. The findings showed that the technologists were more satisfied than the radiologists were with using the PACS. Interestingly, there was a significant relationship between the perceived benefits of the PACS and the willingness of users to continue using it. It was also noteworthy that the problems associated with the PACS’s integration with the RIS were the result of disorganized workflow.
The results of the study revealed that the users’ demographic data, including computer experience, had no influence on their response patterns, being insignificant determinants of their predilection or preference for the PACS in enhancing their work efficiency. These findings were consistent with the study’s results on PACS acceptance[7], but contradicted with the results of earlier studies that reported the significant influence of age and gender on users’ choices concerning information technology, such as computer use patterns[20][21], particularly to adopting PACS.[3][8]
Perceptions of PACS quality, information, images, and services
The study further revealed that both the radiologists and the technologists were satisfied with the quality of information and images produced and had positive views regarding the use of this technology. The PACS offered the users with the requisite information on a medical case and facilitated the accomplishment of several functions with efficiency and ease in producing high-quality images with precision and clarity. This positive relationship found between users' satisfaction and quality of information and images produced by PACS was consistent with the findings of previous studies.[1][22] The results of the interviews further complemented these findings, with no mention of lost images posing a major problem, due to successful image retrieval by PACS administrators.
The study found that the technologists were more satisfied than the radiologists concerning their current PACS use, attributing their satisfaction to two reasons, which had been confirmed in previous studies[2][6][23]: the technologists achieved their core objectives of using the PACS, including image access, storage, and retrieval; and (2) the radiologists looked beyond these features for additional facilities and functions, such as the PACS being packaged with CAD, teleradiology, or speech recognition functions. As the radiologists had been using the PACS far longer than the technologists had, their understanding and familiarity with the PACS appeared to be relatively higher.
Concerning the quality of the services offered to support PACS technically, the findings showed that both users were satisfied with the technical support provided with regard to the promptness, reliability, and dependability of the services. However, the results of the interviews revealed that the radiologists and the technologists encountered organizational and infrastructure deficiencies. On the technical level, there was frequent breakdown of the system during rush hours; and on organizational level, there was negligence of some receptionists in recording patients’ information from the RIS to the HIS. Interestingly, the respondents still showed satisfaction in confirming the benefits of the PACS over conventional radiology despite some deficiencies, as reportedly addressed in previous studies.[3][22]
Perceptions of the PACS’s impact, including net benefits and user satisfaction
Regarding the PACS’s net benefits, the findings demonstrated that both the radiologists and the technologists had used the PACS to enhance their work productivity with ease due to the swift storage, retrieval, and transfer of images along with reports. These findings were consistent with those reported in previous evaluative studies on the impact of PACS[6][24], confirming that work productivity in regard to the given effort, time, and accuracy of reporting has obviously been improved. Furthermore, the PACS’s benefits were found to have direct implications for user satisfaction, affecting their continued use of the PACS in the future.[16] These previous studies concluded that the more the users agreed with a PACS’s effectiveness in their work, the more they were satisfied and willing to continue using it. The findings of the interviews further confirmed that both types of users benefited from the PACS’s advantages, expressing their readiness toward the technology’s continuous use while looking ahead for additional functions, without deficiencies, which coincided with other studies.[25][26][27]
Limitations
(1) This study was limited to radiologists and radiology technologists and did not involve other health care providers who are responsible for receiving patients’ reports and images. Hence, there is a need for further research that would substantiate the study’s findings by involving other stakeholders using the PACS facility, for the purpose of comparing research outcomes and enhancing the study’s value. (2) The study also did not include socioeconomic and cultural factors, which are significant predictors of IT adoption in the Arab world[7][28][29] in comparison to Western countries. However, the respondents’ willingness to use the PACS was a positive indicator of the technology’s versatility, efficiency, and continuous use. (3) As the study was confined to one general hospital in Kuwait, there is a definitive need for future studies to enhance the study’s scope by including other hospitals where PACSs are being used, for comparative purposes. (4) The study used specific criteria in evaluating IS success; hence, there is a need for using different models and tools for exploring and assessing PACSs and RISs from different dimensions.
Conclusion
Evaluating the applications of imaging informatics, such as PACSs, in hospitals is crucial to ensure the successful implementation of the applications, to identify the systems’ strengths and weaknesses during operation, and to provide the opportunity for further improvements, strengthening the positive elements and minimizing drawbacks. The evaluation of the existing PACS at Mubarak Al-Kabeer teaching hospital led to the successful assessment of the technology’s implications, based on which the study’s conclusions are summarized: (1) the PACS exhibited a positive impact on the radiologists and the technologists in the diagnostic radiology department, significantly enhancing their work efficiency and productivity. Therefore, the impact of the technology was particularly visible in the context of its ability to store and retrieve images quickly, enabling the users to accomplish their tasks swiftly. In addition, the system facilitated the addition of an image to a report, expediting communication with another location with a keystroke; (2) the main concern reported by all the users was the frequent breakdown during rush hours at busy workstations, due to infrastructure deficiency; (3) both the technologists and the radiologists indicated the need for a more-advanced PACS in response to the growing demand of teleradiology, mobile image viewing, and voice recognition features; and (4) evaluating PACS’s success is not confined to the technology itself but also concerns organizational and human factors that could limit the full integration with HIS.
Recommendations
To improve the work on the current PACS and overcome the deficiencies, the following recommendations could be considered at Mubarak Al-Kabeer general hospital: (1) Enhance the capacity of existing servers to accommodate the huge amount of data generated from the massive inflow of patients. (2) Develop an internal policy to facilitate the coordination with the hospital management for organizing hospital workflow with efficiency. This policy should be followed carefully by the department staff for achieving the full benefits of the PACS’s integration with the HIS and the RIS. (3) Offer advanced training courses for fully using the PACS’s functions. (4) Keep a forward-looking eye on future trends of PACS, including teleradiology services, mobile images viewing, speech recognition, and CAD. (5) Hire health informatics specialists for providing the requisite administrative support on account of their knowledge in the field.
Acknowledgments
Special thanks go to all the staff at the radiology department of Mubarak Al-Kabeer Teaching Hospital in Kuwait for their efforts and contributions in making this study successful.
Conflicts of interest
None declared.
References
- ↑ 1.0 1.1 Tzeng, W.S.; Kuo, K.M.; Lin, H.W.; Chen, T.Y. (2013). "A socio-technical assessment of the success of Picture Archiving and Communication Systems: The radiology technologist's perspective". BMC Medical Informatics and Decision Making 13: 109. doi:10.1186/1472-6947-13-109. PMC PMC3849362. PMID 24053458. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3849362.
- ↑ 2.0 2.1 Vest, J.R.; Jung, H.Y.; Ostrovsky, A. et al. (2015). "Image Sharing Technologies and Reduction of Imaging Utilization: A Systematic Review and Meta-analysis". Journal of the American College of Radiology 12 (12 Pt B): 1371-1379.e3. doi:10.1016/j.jacr.2015.09.014. PMC PMC4730956. PMID 26614882. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4730956.
- ↑ 3.0 3.1 3.2 Duyck, P.; Pynoo, B.; Devolder, P. et al. (2010). "Monitoring the PACS implementation process in a large university hospital: Discrepancies between radiologists and physicians". Journal of Digital Imaging 23 (1): 73–80. doi:10.1007/s10278-008-9163-7. PMC PMC3043749. PMID 18956231. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3043749.
- ↑ 4.0 4.1 4.2 Hains, I.M.; Georgiou, A.; Westbrook, J.I. (2012). "The impact of PACS on clinician work practices in the intensive care unit: a systematic review of the literature". JAMIA 19 (4): 506–13. doi:10.1136/amiajnl-2011-000422. PMC PMC3384105. PMID 22323392. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3384105.
- ↑ Bryan, S.; Weatherburn, G.C.; Watkins, J.R.; Buxton, M.J. (1999). "The benefits of hospital-wide picture archiving and communication systems: A survey of clinical users of radiology services". The British Journal of Radiology 72 (857): 469-78. doi:10.1259/bjr.72.857.10505012. PMID 10505012.
- ↑ 6.0 6.1 6.2 Tan, S.L.; Lewis, R.A. (2010). "Picture archiving and communication systems: A multicentre survey of users experience and satisfaction". European Journal of Radiology 75 (3): 406–10. doi:10.1016/j.ejrad.2009.05.008. PMID 19523778.
- ↑ 7.0 7.1 7.2 Aldosari, B. (2012). "User acceptance of a picture archiving and communication system (PACS) in a Saudi Arabian hospital radiology department". BMC Medical Informatics and Decision Making 12: 44. doi:10.1186/1472-6947-12-44. PMC PMC3423046. PMID 22640490. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3423046.
- ↑ 8.0 8.1 Bryan, S.; Weatherburn, G.; Buxton, M. et al. (1999). "Evaluation of a hospital picture archiving and communication system". Journal of Health Services Research and Policy 4 (4): 204-9. doi:10.1177/135581969900400405. PMID 10623035.
- ↑ Moodley, I.; Moodley, S. (2015). "A comparative cost analysis of picture archiving and communications systems (PACS) versus conventional radiology in the private sector". South African Journal of Radiology 19 (1): 634-641. doi:10.4102/sajr.v19i1.634.
- ↑ Mackinnon, A.D.; Billington, R.A.; Adam, E.J. et al. (2008). "Picture archiving and communication systems lead to sustained improvements in reporting times and productivity: Results of a 5-year audit". Clinical Radiology 63 (7): 796-804. doi:10.1016/j.crad.2007.12.015. PMID 18555038.
- ↑ van de Wetering, R.; Batenburg, R.; Versendaal, J. et al. (2006). "A balanced evaluation perspective: Picture archiving and communication system impacts on hospital workflow". Journal of Digital Imaging 19 (Suppl 1): 10. doi:10.1007/s10278-006-0628-2. PMC PMC3045172. PMID 16763932. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3045172.
- ↑ Creswick, N.; Hains, I.M.; Westbrook, J.I. (2011). "Innovation in intensive care nursing work practices with PACS". Studies in Health Technology and Informatics 169: 402–6. doi:10.3233/978-1-60750-806-9-402. PMID 21893781.
- ↑ van de Wetering, R.; Batenburg, R. (2014). "Towards a theory of PACS deployment: An integrative PACS maturity framework". Journal of Digital Imaging 27 (3): 337–50. doi:10.1007/s10278-013-9671-y. PMC PMC4026462. PMID 24448919. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4026462.
- ↑ 14.0 14.1 Friedman, C.P.; Wyatt, J. (2006). Evaluation Methods in Biomedical Informatics. Springer-Verlag New York. pp. 386. doi:10.1007/0-387-30677-3. ISBN 9780387258898.
- ↑ Mansoori, B.; Erhard, K.K.; Sunshine, J.L. (2012). "Picture Archiving and Communication System (PACS) implementation, integration & benefits in an integrated health system". Academic Radiology 19 (2): 229–35. doi:10.1016/j.acra.2011.11.009. PMID 22212425.
- ↑ 16.0 16.1 16.2 Paré, G.; Lepanto, L.; Aubry, D.; Sicotte, C. (2005). "Toward a multidimensional assessment of picture archiving and communication system success". International Journal of Technology Assessment in Health Care 21 (4): 471–9. doi:10.1017/S0266462305050658. PMID 16262970.
- ↑ DeLone, W.H.; McLean, E.R. (1992). "Information Systems Success: The Quest for the Dependent Variable". Information Systems Research 3 (1): 60–95. doi:10.1287/isre.3.1.60.
- ↑ DeLone, W.H.; McLean, E.R. (2003). "The DeLone and McLean Model of Information Systems Success: A Ten-Year Update". Journal of Management Information Systems 19 (4): 9–30. doi:10.1080/07421222.2003.11045748.
- ↑ Joshi, V.; Narra, V.R.; Joshi, K. (2014). "PACS administrators' and radiologists' perspective on the importance of features for PACS selection". Journal of Digital Imaging 27 (4): 486-95. doi:10.1007/s10278-014-9682-3. PMC PMC4090402. PMID 24744278. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4090402.
- ↑ Ward, R.; Stevens, C.; Brentnall, P.; Briddon, J. (2008). "The attitudes of health care staff to information technology: A comprehensive review of the research literature". Health Information and Libraries Journal 25 (2): 81-97. doi:10.1111/j.1471-1842.2008.00777.x. PMID 18494643.
- ↑ Adeleke, I.; Adejoke, A.; Achinbee, M. et al. (2015). "ICT knowledge, Utilization and Perception among Healthcare Providers at National Hospital Abuja, Nigeria". American Journal of Health Research 3 (1-1): 47-53. doi:10.11648/j.ajhr.s.2015030101.173.
- ↑ 22.0 22.1 Sicotte, C.; Paré, G.; Bini, K.K. et al. (2010). "Virtual organization of hospital medical imaging: A user satisfaction survey". Journal of Digital Imaging 23 (6): 689-700. doi:10.1007/s10278-009-9220-x. PMC PMC3046687. PMID 19588196. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3046687.
- ↑ Folio, L.R.; Nelson, C.J.; Benjamin, M. et al. (2015). "Quantitative Radiology Reporting in Oncology: Survey of Oncologists and Radiologists". American Journal of Roentgenology 205 (3): W233-43. doi:10.2214/AJR.14.14054. PMID 26295661.
- ↑ Sevenster, M.; Travis, A.R.; Ganesh, R.K. et al. (2015). "Improved efficiency in clinical workflow of reporting measured oncology lesions via PACS-integrated lesion tracking tool". American Journal of Roentgenology 204 (3): 576-83. doi:10.2214/AJR.14.12915. PMID 25714288.
- ↑ Hsiao, J.L.; Chen, R.F. (2016). "Critical factors influencing physicians' intention to use computerized clinical practice guidelines: An integrative model of activity theory and the technology acceptance model". BMC Medical Informatics and Decision Making 16: 3. doi:10.1186/s12911-016-0241-3. PMC PMC4715302. PMID 26772169. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4715302.
- ↑ Liu, C.F.; Cheng, T.J. (2015). "Exploring critical factors influencing physicians' acceptance of mobile electronic medical records based on the dual-factor model: A validation in Taiwan". BMC Medical Informatics and Decision Making 15: 4. doi:10.1186/s12911-014-0125-3. PMC PMC4333263. PMID 25889506. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4333263.
- ↑ Floyd, D.M.; Trepp, E.R.; Ipaki, M.; Ng, C.K. (2015). "Study of Radiologic Technologists' Perceptions of Picture Archiving and Communication System (PACS) Competence and Educational Issues in Western Australia". Journal of Digital Imaging 28 (3): 315–22. doi:10.1007/s10278-014-9765-1. PMC PMC4441692. PMID 25561072. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4441692.
- ↑ Ray, K.N.; Felmet, K.A.; Hamilton, M.F. et al. (2017). "Clinician Attitudes Toward Adoption of Pediatric Emergency Telemedicine in Rural Hospitals". Pediatric Emergency Care 33 (4): 250-257. doi:10.1097/PEC.0000000000000583. PMID 26785087.
- ↑ Straub, D.; Loch, K.; Hill, C. (2001). "Transfer of Information Technology to the Arab World: A Test of Cultural Influence Modeling". Journal of Global Information Management 9 (4): 6–28. doi:10.4018/jgim.2001100101.
Abbreviations
CAD: computer-assisted diagnosis
HIS: health information system
ID: identification
IS: information system
PACS: picture archiving and communication System
RIS: radiology information system
Notes
This presentation is faithful to the original, with only a few minor changes to presentation. In several cases the PubMed ID was missing and was added to make the reference more useful.
Per the distribution agreement, the following copyright information is also being added:
©Ali Jassem Buabbas, Dawood Ameer Al-Shamali, Prem Sharma, Salwa Haidar, Hamza Al-Shawaf. Originally published in JMIR Medical Informatics (http://medinform.jmir.org), 15.06.2016.